Bye Jonas Waldenström
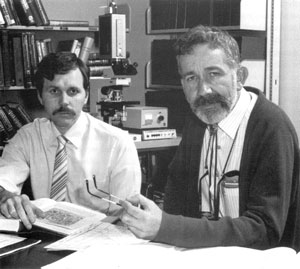
Of all inhospitable places, your stomach is one of the most hostile. Made to dissolve the food you eat, this interior body chamber is a veritable hell and any bug aiming to infect your intestines needs to survive a long hydrochloric acid bath. Thus, your stomach is a barren, acid wasteland. Or, at least that was what everyone believed until two Australian researchers – Barry Marshall and Robin Warren – entered the limelight. The duo repeatedly found curved rod-shaped bacilli in gut biopsies from humans with gastritis, and speculated that it may be the causative agent behind this and other gut diseases.
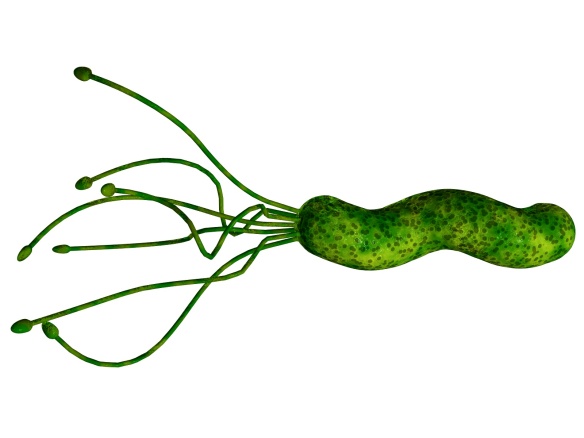
Say hello to Mr Helicobacter pylory! He is a curved rod with a bunch of flagellae. He likes to live in your stomach.
At first no one believed them; their findings were directly contradicting the existing paradigm. They were criticized, even ridiculed. ‘Something living in the stomach?! Bah, humph! Contamination, dear fellows, CONTAMINATION!’ However, quite soon it became clear that Marshall and Warren were right. Even more so, the bug – nowadays known as Helicobacter pylori – not only thrived in the stomach, it was also a pathogen associated with important human scourges as peptic ulcers and stomach cancers. Suddenly there was a biological target to hit in order to tackle these diseases – a major finding that has changed the lives of many, many people in the world. In recognition of their contribution to science, Marshall and Warren were awarded the Nobel Prize in Physiology or Medicine in 2005. Marshall also used himself as an experimental model to test the causality of Helicobacter pylori and gastritis. He simply swallowed a culture from a Petri dish and, yes, he developed the nasty symptoms! (As well as bad breath, mostly noted by his mother). Although not generally recommendable, it served a point and the Koch’s postulates were met.
Last week I attended the CHRO 2013 meeting in Aberdeen, Scotland. This biannual meeting brings together the biggest brains on Campylobacter, Helicobacter, and related organisms, and is a very nice melting pot. Here you can meet and discuss with friends and foes from the four corners of the world, and peek on the latest news from the research front. I really like these meetings, particularly because of the friendly attitude. This time the organizers wanted an historical perspective, as it is approximately 30 years since both Campylobacter and Helicobacter were recognized as pathogens (and also since the professors that was there at the start are soon to retire). I am generally a Campylobacter-guy (and flu-guy), and have only published one paper on Helicobacter. But I find the bug intriguing. Not only because of the link to diseases, but also their limited transmission (within families mostly, due to kissing, or perhaps fecal-oral transmission) that even make it possible to use them as a proxy of population origin. Make a map of Helicobacter relatedness and it will give a nice map of the world. It is also a bug that doesn’t cause disease quick, or at all. In fact, more than half of the world’s population is infected with Helicobacter, and the vast majority will never experience any symptoms. It is quite likely that you (or me) are carrying this bacterium right now, but that we only will have symptoms if our equilibrium is altered, by prolonged stress or other conditions.
The field has come a long way in the three decades of research. A success story really. Now we can fairly easily cure Helicobacter infections with different antibiotic therapies. Severe, bleeding peptic ulcers are nowadays rare. However, Helicobacter as a cause of gastric cancer is still a major issue. In fact, this bug is one of the top carcinogenic microorganisms we know of (together with human papilloma virus and Epstein-Barr virus) and stomach cancer is one of the most common cancers in the world responsible for roughly 9% of all cancers. So how can Helicobacter cause cancer? This isn’t all settled yet, and is likely multifaceted. A lot of the pathogenesis involved, including the different biomolecules and pathways, is so now targeted in research, and also how differences in lifestyle and genetics affect the likelihood of developing cancer.
The incidence of stomach cancer is highest in Asia, and there are now plans to perform large-scale eradication of Helicobacter in the human population in Japan. The tools are there, and now the question is if we can achieve the goal in practice? The infection can be detected with simple breath tests and only those persons that are positive need to get therapy. However, nuking away Helicobacter at large scale can come with a cost – and possibly a rebound. In essence, this is a biological manipulation of an ecosystem – bug and human in this case – through a mediator that is antibiotics. Let’s face it: our track record in fiddling with nature isn’t great. Consider the introduction of Aga toads in Australia, water lilies in Africa and many, many other examples of exogenous fauna manipulations. As regards diseases, despite a century of medical invention, drug discoveries and vaccine developments we have actually only terminated one single disease: smallpox. In many other cases we have just given ourselves respite while resistance is slowly developing.
The problem is two-fold. First, antibiotic therapy imposes an enormous selection pressure. Any bug out there with any type of resistance to the drug will be at an advantage and can increase in frequency in the population. Given the generation time of bacteria vs. men, the bugs are usually those running the shots. (For an excellent view of evolutionary medicine please view Professor Andrew F. Read’s TED-talk.) The harder we hit, the higher the gain is for the mutants. And if therapy coverage isn’t good enough foci in the population of humans may still carry the bacterium and transmit it back. Helicobacter is a bit special, I admit as much, and perhaps easier to eradicate than other diseases. Still, the question is whether the limited distribution of the bacterium, the efficacy of therapy, and stringent follow-up is enough to get rid of Helicobacter, or, whether one is creating super-resistant bacteria that will increase in frequency? We don’t want to have any Darwinian-demon helicobacters.
The second problem is the ‘what if’-dilemma. Okay, Helicobacter pylori is for certain a pathogen. But it isn’t causing disease in all humans, rather in specific persons under certain environmental conditions. Stress, coffee and diet will influence your gut, and the ability for Helicobacter to cause harm. But what if Helicobacter is also providing some benefits to us? Something we are not even aware of. Maybe they outcompete other potential stomach colonizing bacteria? A particular worry could be the >20 other Helicobacter species described in other animal species (of which some have also been detected in humans). What if they find a niche in humans in the post-Helicobacter pylori world? Are they big velicoraptors waiting in the shadows?
Time will tell. And risks and benefits need to be weighed. Undoubtedly, an effective strike at a bug is really tempting if it will reduce the incidence of gastric cancer in the years to come.
Waldenström, J., On, S.LW., Ottvall, R., Hasselquist, D., Harrington, C.S. & Olsen, B. 2003. Avian reservoirs and zoonotic potential of the emerging human pathogen Helicobacter canadensis. Applied and Environmental Microbiology 69: 7523-7526.